Personality Disorders: The Clusters, The Facts, & The Relief
Personality Disorders and Intellectual Disabilities are considered an Axis II disorder by the DSM-IV, which provides a detailed diagnosis of a host of illnesses and explains all of the acute symptoms.
It is exceedingly important to note that most individuals with an Axis I Mood Disorder, such as Major Depressive disorder and Bipolar Disorder. It is prevalent for people to suffer from both, which significantly exacerbates and complicates both illnesses. Most have at least three.
These are some psychiatric conditions that may cause long-life problems in an individual’s relationships and work. An individual with a personality disorder typically behaves very differently from what society expects of them. The World Health Organization classifies personality disorders as mental disorders on Axis II.
Personality is defined as the enduring behavioral mental traits that distinguish human beings. Hence, a personality disorder is defined as the difficulty to experience some problems in cognition, emotiveness, control of impulses, or interpersonal functioning.
There are many causes of personality disorders that vary from one individual to the other. They may include personal life experiences, incidences of abuse, or trauma experienced in one’s life.
One of the most significant antecedent risks of personality disorders is child neglect and abuse in earlier stages of life. Research has shown that many children who were either physically or sexually abused showed the most significant incidences of the patterns of psychopathology.
Common Personality Disorders
Below is a brief description of some of the common personality disorders:
- Avoidant- these people fail to do tasks that will even benefit them
- Antisocial- they don’t want to associate with others
- Histrionic- they make a significant faction out of something minimal—sometimes referred to as drama queens
- Borderline- people with this personality disorder tend to behave immaturely and stay in crisis most of the time
- Narcissistic- this is a person who is in love with themselves and tends to be arrogant most of the time
- Paranoid- this is a person who is always afraid that something or somebody is out to get them
- Dependent- these are people who always depend on others for everything and can’t make a decision on their own
- Schizotypal- this is a person who has problems with their thoughts, appearance, and even relationships with others
- Obsessive-compulsive- such people tend to have some ideas and feelings followed by actions that don’t relate to them in any way
- Schizoid- they live in complete social isolation and behave differently from other people
So, What Is An Axis II Personality Disorder?
The most pervasive symptoms of Personality Disorders include frequent mood swings, unhealthy relationships, a propensity toward isolation, angry outbursts, suspicious and paranoia, difficulty making (and especially in retaining) friendship and romantic attachments, a need for instant gratification, poor impulsive control, an alcohol or substance abuse. This is one of the factors that makes correctly diagnosing an Axis II disorder (or certain Axis II disorders, for that matter), as the traits tend to overlap.
Other characteristics frequently seen in Axis I and Axis II conditions are a particular class of mental exhaustion and emotionality scorned by precipitous societal stigma; it can make the chronic illnesses seem unmanageable and even beyond hope.
Many more progressive doctors find the term in and of itself to be a problem (I cannot overstate how many times I have heard people who’ve been diagnosed with a Personality Disorder say, “It’s my illness; my personality is me!”). According to a doctor at the Mayo Foundation for Medical Education and Research (MFMER):
[T]he diagnosis “personality disorder’ should be replaced by the diagnosis “adaptation disorders’. This reflects the real nature of the disorder more accurately, and is likely to reduce the stigmatizing component of the personality disorder diagnosis as it places emphasis on positive efforts to improve adaptation. The suggested revisions of the personality disorder diagnosis and dimensional approach to these disorders are likely to advance treatment and research—we discuss these aspects in some detail.
The most commonly diagnosed Axis II disorders are as follows:
- Antisocial
- Avoidant
- Borderline
- Dependent
- Histrionic
- Narcissistic
- Obsessive-Compulsive
- Paranoid
- Schizoid
- Schizotypal
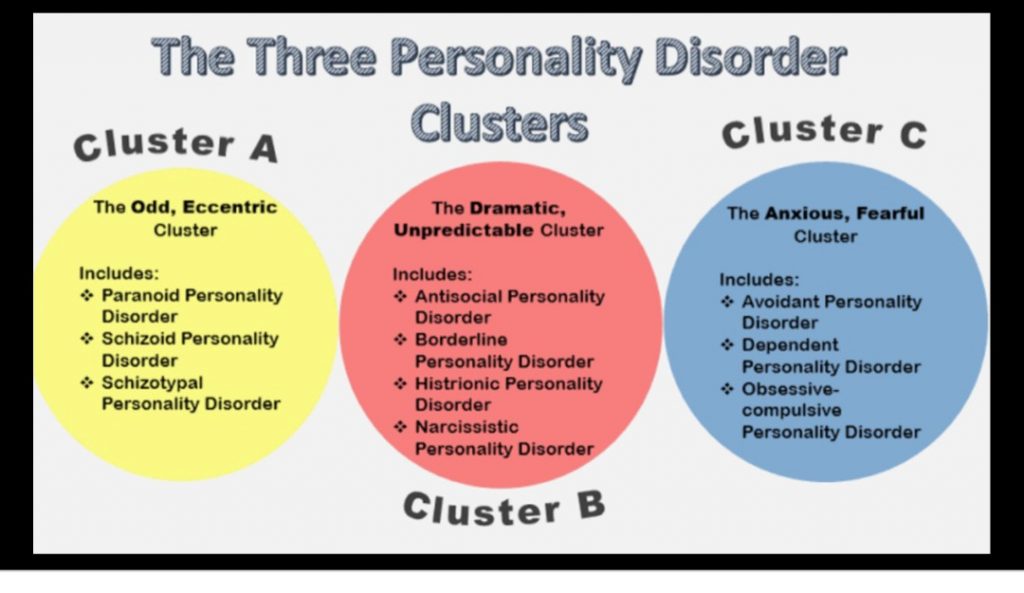
These disorders are grouped into three “clusters” (A, B, and C) based on similarities in the symptoms. Having one does not preclude you from having a secondary Axis II disorder; instead, it increases your chances, which is why therapy is essential for anyone with a chronic behavioral health illness, regardless of what it is or how many.
Traditional psychotherapy, family therapy, Cognitive Behavioral Therapy (CBT), and Dialectical Behavioral Therapy (DBT), to name four quite popular types, have been significantly proven successful at alleviating some of the most acute characteristics.
Cluster A
Personality disorders are grouped by illnesses where odd, eccentric thinking, or behavior are central and prominent. This includes Paranoid Personality Disorder (distrust of others, believing others are trying to harm you, emotional detachment, and hostility);
Schizoid Personality Disorder (lack of interest in social relationships, limited ranged emotion expression, inability to pick up so-called “normal” societal cues, and appearing indifferent to people, places, and events);
Schizotypal Personality Disorder (abnormal thinking, beliefs, or behavior, sensory-perceptual alterations, discomfort in close-knit relationships, flat or inappropriate emotional responses, indifference toward others, believing that messages intended only for you are in plain sight within public forums or even speeches, and engaging in “magical thinking, such as the ability of others to read and influence your thoughts).
Cluster B
Personality disorders are often classified due to the individual’s dramatic and overly emotional thoughts and actions. This includes Antisocial Personality Disorder (which used to be called Sociopathic, and is typified by a frequent disregard for others, constant lying and stealing, recurring difficulties with the law, repeatedly violating the rights of others by using aggressive, often violent behavior, and a prevailing disregard for the safety of themselves and others);
Borderline Personality Disorder (impulsive/risky behavior, volatile/volatile relationships, instability concerning mood, self-injurious acts, and suicidal behavior);
Histrionic Personality Disorder (classified as someone who is constantly seeking attention and has a prevailing concern with their physical appearance, extreme sensitivity to the approval [or disapproval] of others, and a chronically unstable mood); and
Narcissistic Personality Disorder (includes fantasizing about power, success, and attractiveness, exaggerating one’s achievements or talents, the expectation of constant praise and admiration, and continually failing to recognize the emotions and emotional needs of other people).
Cluster C
Personality disorders are often typified by anxious, fearful thinking/behavior. Avoidant Personality Disorder is comprised of significant hypersensitivity toward criticism or rejections, feeling inadequate and timid, and thereby very shy in social settings. A person with this Axis II disorder would most likely have intense social anxiety, but also have a grave dislike for social isolation, making it a highly complex illness to treat);
Dependent Personality Disorder (commonly reflected as an excessive dependence on and submissiveness to others, a desire/need to be taken care of, tolerance of poor or even abusive treatment, and the urgent need to begin a new romantic relationship as soon as one concludes);
Obsessive-Compulsive Personality Disorder (this disorder usually entails a preoccupation with orderliness and rules, extreme and unhealthy perfectionism, the desire to be in control, an inability or great challenge in discarding broken objects, and a general lack of flexibility in toto).
Please note: Obsessive Compulsive Disorder (OCD) is not the same as Obsessive Compulsive Personality Disorder, which is a class of anxiety disorder.
Is There Any Hope In Overcoming A Personality Disorder?
In a word: yes! Firstly, getting a correct diagnosis from a knowledgeable and caring psychiatrist is essential, followed by adherence to your safety plan, which may or may not include medication, but should include therapy. The best class can be sorted between you and your doctor (and perhaps a conversation with allies, including family and friends). You can even engage in several yourself to decide which you feel you will benefit most from and finding out what type the majority of people with your illness(es) utilize and why.
Additionally, there are now many mood stabilizers, antidepressants, anti-anxiety, and antipsychotic medications that have been proven to aid significantly with helping people recover, so long as they remain dedicated to their treatment and live a healthier lifestyle.
In instances where individuals are in grave danger of harming themselves or others or have developed psychotic conditions, relatively brief psychiatric hospitalizations (usually 72 hours to three or four weeks [the latter when receiving, for example, ECT or severe medication adjustments, which mandates hospital stays for safety and monitoring).
Cognitive Behavioral Therapy (CBT) is one of several modes of care used to treat personality disorders. Dialectical Behavioral Therapy (DBT) is built upon this model, adding Zen practices (e.g., mindfulness) and the Hegelian principle of the analytic process.
There are different modalities for the treatment of these disorders and others:
- Individual Psychotherapy- this is the most common form of treatment where the individual undergoes the standard treatment.
- Family Therapy- it may include couples and sometimes children together
- Group Therapy- all the people categorized with the same personality disorder are placed under similar treatment conditions
- Psychological Education- it is used as an additional form of treatment to the primary methods
- Self Help Groups- they help provide people living with personality disorders with powerful resources for treatment and overall well being
- Psychiatric Medications- the symptoms of the personality disorder or other co-occurring conditions are treated.
- Milieu Therapy- this is a group-based residential approach to treating these psychological disorders. It could include therapeutic communities.
Due to the rising number of people with personality disorders in the world these days, there are many NGOs through various means such as websites trying to sensitize people with personality disorders on the approach to take.
It would be best to get better because you know you can (e.g., roughly a decade of participating in DBT will reduce or even eliminate approximately 86% of BPD cases), and give yourself that new life starting with some small steps (and soon!). Try to maintain your medical care, exercise, and activity (and less social isolation, as hard as that is!), making healthier food and drink choices, learn all about your illness(es), and pay attention to your triggers and warning signs to better understand when the pain is most profound; that way, you can create a solid safety plan, and get into more intensive treatment right away.
Use your expertise to defeat these diseases. And remember: it is imperative to learn some relaxation techniques and stress management (deep breathing is a great way to begin, and I love Ashtanga yoga); perhaps join a support group (contrary to everything I’d assumed, DBT group therapy has always been transformative and empowering); and, of course, be kind and gentle with yourself.
Trending Health Topics
- ADHD
- Allergies
- Arthritis
- Bipolar Disorder
- Bunions
- Car Accidents
- Chron's Disease
- Common Cold
- COPD
- Depression
- Dry Skin
- Dry throat
- Eczema
- Fungal Infection
- GERD
- HIV/AIDS
- Hypertension
- Irritable Bowel Syndrome (IBS)
- Multiple Sclerosis
- Osteoarthritis
- Psoriasis
- Rheumatoid Arthritis
- Skin Disorders
- strep throat
- Type 2 Diabetes
- Uncategorized