Inflammatory bowel disease (IBD) involves chronic inflammation of all or part of your digestive tract. IBD primarily includes ulcerative colitis and Crohn’s disease. Both usually involve severe diarrhea, pain, fatigue and weight loss. IBD can be debilitating and sometimes leads to life-threatening complications.
Ulcerative colitis (UL-sur-uh-tiv koe-LIE-tis) is an inflammatory bowel disease that causes long-lasting inflammation and sores (ulcers) in the innermost lining of your large intestine (colon) and rectum.
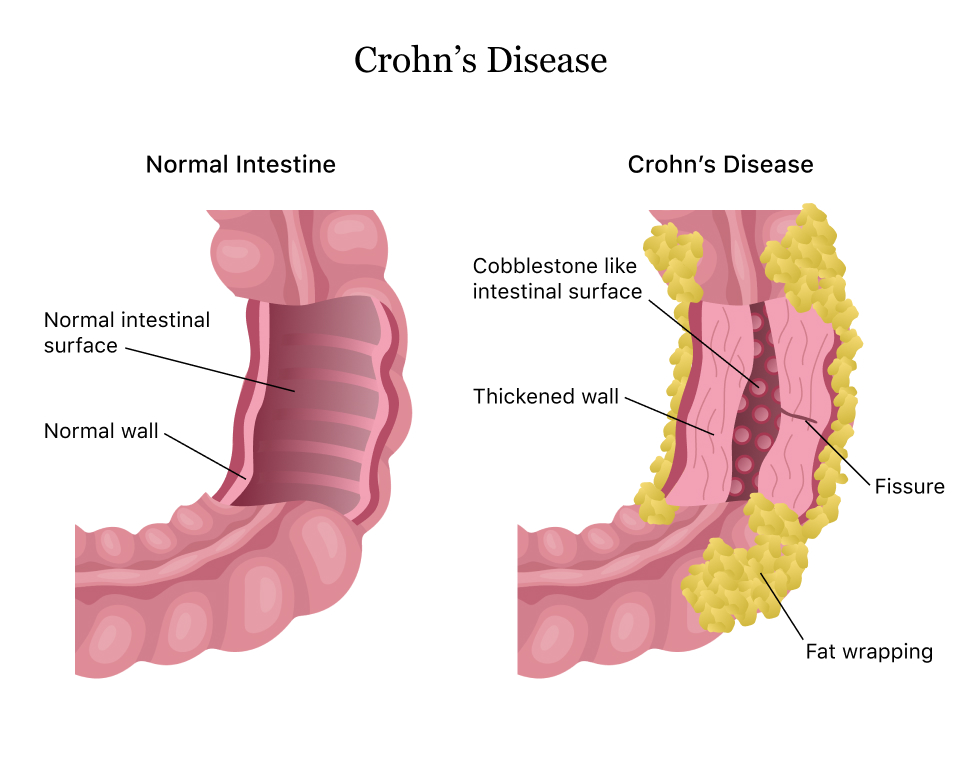
Crohn’s disease is an IBD that cause inflammation of the lining of your digestive tract. In Crohn’s disease, inflammation often spreads deep into affected tissues. The inflammation can involve different areas of the digestive tract — the large intestine, small intestine or both.
Collagenous (kuh-LAJ-uh-nus) colitis and lymphocytic colitis also are considered inflammatory bowel diseases but are usually regarded separately from classic inflammatory bowel disease.
Symptoms
Inflammatory bowel disease symptoms vary, depending on the severity of inflammation and where it occurs. Symptoms may range from mild to severe. You are likely to have periods of active illness followed by periods of remission.
Signs and symptoms that are common to both Crohn’s disease and ulcerative colitis include:
- Diarrhea. Diarrhea is a common problem for people with IBD.
- Fever and fatigue. Many people with IBD experience a low-grade fever. You may also feel tired or have low energy.
- Abdominal pain and cramping. Inflammation and ulceration can affect the normal movement of contents through your digestive tract and may lead to pain and cramping. You may also experience nausea and vomiting.
- Blood in your stool. You might notice bright red blood in the toilet bowl or darker blood mixed with your stool. You can also have bleeding you don’t see (occult blood).
- Reduced appetite. Abdominal pain and cramping, as well as inflammation, can affect your appetite.
- Unintended weight loss. You may lose weight and even become malnourished because you cannot properly digest and absorb food.
Types
Ulcerative colitis is classified according to the location of inflammation and severity of symptoms:
- Ulcerative proctitis. Inflammation is confined to the area closest to the anus (rectum), and rectal bleeding may be the only sign of the disease. This form of ulcerative colitis tends to be the mildest.
- Proctosigmoiditis. Inflammation involves the rectum and sigmoid colon (lower end of the colon). Signs and symptoms include bloody diarrhea, abdominal cramps and pain, and an inability to move the bowels in spite of the urge to do so (tenesmus).
- Left-sided colitis. Inflammation extends from the rectum up through the sigmoid and descending colon. Signs and symptoms include bloody diarrhea, abdominal cramping and pain on the left side, and unintended weight loss.
- Pancolitis. Pancolitis often affects the entire colon and causes bouts of bloody diarrhea that may be severe, abdominal cramps and pain, fatigue, and significant weight loss.
- Acute severe ulcerative colitis. Previously called fulminant colitis, this rare form of colitis affects the entire colon and causes severe pain, profuse diarrhea, bleeding, fever and inability to eat.
Crohn’s disease may involve inflammation in different parts of the digestive tract in different people. The most common areas affected are the last part of the small intestine (ileum) and the colon. Inflammation may be confined to the bowel wall, which can lead to narrowing from inflammation or scarring or both (fibrostenosis), or may tunnel through the bowel wall (fistula). Narrowing may lead to a blockage (obstruction). Obstructions, stenosis and fistulas are not associated with ulcerative colitis.
When to see a doctor
See your doctor if you experience a persistent change in your bowel habits or if you have any of the signs and symptoms of inflammatory bowel disease. Although inflammatory bowel disease usually isn’t fatal, it’s a serious disease that, in some cases, may cause life-threatening complications.
Causes
The exact cause of inflammatory bowel disease remains unknown. Previously, diet and stress were suspected, but now doctors know that these factors may aggravate but don’t cause IBD.
One possible cause is an immune system malfunction. When your immune system tries to fight off an invading virus or bacterium, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too. Heredity also seems to play a role in that IBD is more common in people who have family members with the disease. However, most people with IBD don’t have this family history.
Risk factors
- Age. Most people who develop IBD are diagnosed before they’re 30 years old. But some people don’t develop the disease until their 50s or 60s.
- Race or ethnicity. Although whites have the highest risk of the disease, it can occur in any race. If you’re of Ashkenazi Jewish descent, your risk is even higher.
- Family history. You’re at higher risk if you have a close relative — such as a parent, sibling or child — with the disease.
- Cigarette smoking. Cigarette smoking is the most important controllable risk factor for developing Crohn’s disease. However, smoking may provide some protection against ulcerative colitis. The overall health benefits of not smoking make it important to try to quit.
- Isotretinoin use. Isotretinoin (Amnesteem, Claravis, Sotret; formerly Accutane) is a medication sometimes used to treat scarring cystic acne or acne. Some studies suggest it may be a risk factor for IBD, but a clear association between IBD and isotretinoin has not been established.
- Nonsteroidal anti-inflammatory medications. These include ibuprofen (Advil, Motrin IB, others), naproxen sodium (Aleve, Anaprox), diclofenac sodium (Voltaren, Solaraze) and others. These medications may increase the risk of developing IBD or worsen disease in people who have IBD.
- Where you live. If you live in an urban area or in an industrialized country, you’re more likely to develop IBD. Therefore, it may be that environmental factors, including a diet high in fat or refined foods, play a role. People living in northern climates also seem to be at greater risk.
Complications
Crohn’s disease may lead to one or more of the following complications:
- Inflammation. Inflammation may be confined to the bowel wall, which can lead to diarrhea and bleeding. Inflammation can also lead to scarring and narrowing (stenosis) or may spread through the bowel wall (fistula).
- Bowel obstruction. Crohn’s disease affects the full thickness of the intestinal wall. Over time, parts of the bowel can thicken and narrow, which may block the flow of digestive contents. You may require surgery to remove the diseased portion of your bowel.
- Ulcers. Chronic inflammation can lead to open sores (ulcers) anywhere in your digestive tract, including your mouth and anus, and in the genital area (perineum).
- Fistulas. Sometimes ulcers can extend completely through the intestinal wall, creating a fistula — an abnormal connection between different body parts. Fistulas can develop between your intestine and skin or between your intestine and another organ. Fistulas near or around the anal area (perianal) are the most common kind.
- When fistulas develop in the abdomen, food may bypass areas of the bowel that are necessary for absorption. Fistulas may occur between loops of bowel, into the bladder or vagina, or out through the skin, causing continuous drainage of bowel contents to your skin.
- In some cases, a fistula may become infected and form an abscess, which can be life-threatening if not treated.
- Anal fissure. This is a small tear in the tissue that lines the anus or in the skin around the anus where infections can occur. It’s often associated with painful bowel movements and may lead to a perianal fistula.
- Malnutrition. Diarrhea, abdominal pain and cramping may make it difficult for you to eat or for your intestine to absorb enough nutrients to keep you nourished. It’s also common to develop anemia due to low iron or vitamin B12 caused by the disease.
- Colon cancer. Having Crohn’s disease that affects your colon increases your risk of colon cancer. General colon cancer screening guidelines for people without Crohn’s disease call for a colonoscopy every 10 years beginning at age 50. However, depending on how long you have had Crohn’s disease and how much of your colon is involved, you may need a colonoscopy as often as every one to two years. Ask your doctor how often you should have a colonoscopy.
- Other health problems. Crohn’s disease can cause problems in other parts of the body, such as inflammation of the eyes, skin or joints; anemia; osteoporosis; inflammation of the liver or bile ducts; and delayed growth or sexual development in children.
- Medications. Certain medications for Crohn’s disease that act by blocking functions of the immune system are associated with a small risk of developing cancers such as lymphoma and skin cancers. They also increase risk of infection.
- Corticosteroids can be associated with a risk of osteoporosis, bone fractures, cataracts, glaucoma, diabetes and high blood pressure. Work with your doctor to determine risks and benefits of medications.
Possible complications of ulcerative colitis include:
- Severe bleeding
- A hole in the colon (perforated colon)
- Severe dehydration
- Liver disease (rare)
- Bone loss (osteoporosis)
- Inflammation of your skin, joints and eyes
- Sores in the lining of your mouth
- An increased risk of colon cancer
- A rapidly swelling colon (toxic megacolon)
- Increased risk of blood clots in veins and arteries