
How COPD Affects Your Life
How COPD affects your life depends on how far it has progressed and how severe your
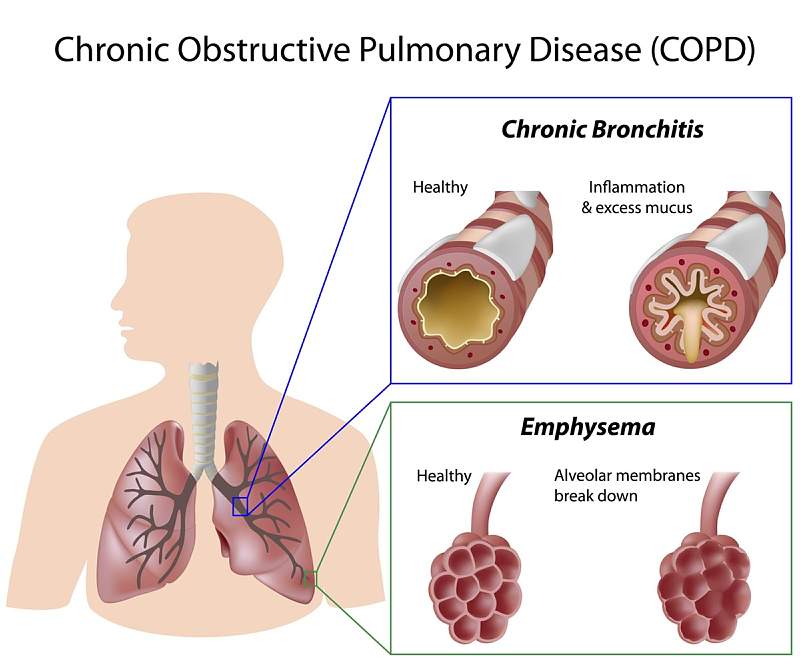
Tobacco smoking is the most common cause for many leading diseases. The other factors such as air pollution and genetics played a smaller role. In the developing world one of the common sources of air pollution is from poorly vented cooking and heating fires. Long term exposure to these irritants causes an inflammatory response in the lungs resulting in narrowing of the small airways and breakdown of lung tissue and lung diseases like COPD. Chronic obstructive pulmonary disease also known as chronic obstructive lung disease and chronic obstructive airway disease. Most people with chronic bronchitis have COPD. COPD is a lung disease that makes it hard to breathe. It is caused by damage to the lungs over many years, usually from smoking. COPD is often a mix of two diseases
There are several things that may increase risk of developing chronic obstructive pulmonary disease (COPD) many of which can be avoided. It can be reduced by not smoking and avoiding exposure to certain substances at work.
Smoking cessation – Stopping smoking is the most effective way for people with COPD to help themselves feel better and is the only proven way to reduce the rate of decline in lung function. Stopping smoking at an early stage of the disease makes a huge difference. Any damage already done to the airways cannot be reversed, but giving up smoking can slow the rate at which the condition worsens. If COPD is in the early stages and symptoms are mild, no other treatments may be needed. Even people with fairly advanced COPD are likely to benefit from quitting, which may prevent further damage to the airways.
Lung therapies
Surgery – Surgery is an option for some people with some forms of severe emphysema
Inhalers

How COPD affects your life depends on how far it has progressed and how severe your
Medical Referral | Accident Attorney Referrals
Filter out the noise and nurture your inbox with health and wellness advice that’s inclusive and rooted in medical expertise.
MedicalReferral.com does not provide medical advice, diagnosis, or treatment.